Our ServicesCervical Canal Stenosis
Cervical stenosis refers to the narrowing of the spinal canal in the neck area, which can compress the spinal cord or nerve roots. This condition can cause symptoms typical of cervical radiculopathy (nerve root pressure) or cervical myelopathy (spinal cord pressure). Most commonly seen in individuals over the age of 50, cervical stenosis may result from age-related degeneration, trauma, inflammation, herniated disk, or tumors.

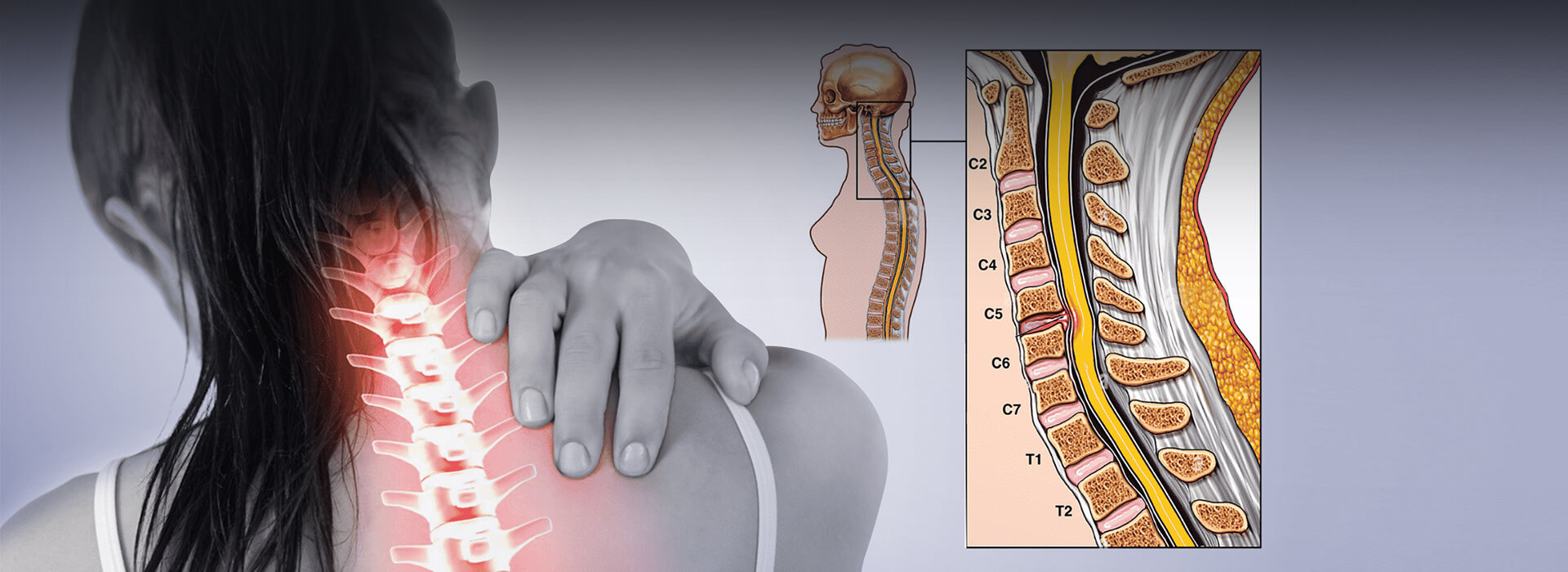
Relevant Anatomy
Understanding the anatomy of the cervical spine is essential for diagnosing and managing cervical stenosis:

Cervical Vertebrae (C1-C7)
The top seven vertebrae in the spine; C1 (atlas) and C2 (axis) are specially designed to allow head motion.

Spinal Canal
The hollow channel within the vertebrae that protects the spinal cord. In stenosis, this space becomes constricted.

Spinal Cord
Extends through the spinal canal; occupies a significant portion of the canal (around 50% at C1 and up to 75% at C6).

Intervertebral Discs
Located between vertebrae, these discs act as shock absorbers. Degeneration or herniation can contribute to narrowing.

Ligaments
Thickening of the ligamentum flavum, among others, can add to canal narrowing.

Osteophytes (Bone Spurs)
These form due to joint degeneration and can encroach on the canal space.

Facet Joints
Arthritic changes here can reduce space within the spinal canal.

Nerve Roots
Emerge through foramina; these can become compressed and lead to radiculopathy.
Understanding how these components interact is key to recognizing how and why symptoms develop.
When conservative  care needs
care needs
a specialist’s touch.
touch.
Disease MechanismCervical stenosis usually arises from a combination of factors, including:
Direct compression of the spinal cord by bony outgrowths (osteophytes) and thickened ligaments.
Reduced blood flow to the spinal cord due to compressed blood vessels, which may result in ischemia.
Herniated disk that cause repeated irritation to the spinal cord or nerve roots during movement, particularly if the spine is unstable.
Cervical segments C5-C6 and C6-C7 are most commonly involved.
EpidemiologyHere’s how cervical stenosis presents across populations:
Affects approximately 4.9% of adults, with prevalence increasing with age (6.8% over 50 and 9% over 70).
Slight male predominance.
Some studies suggest a higher incidence in individuals of white ethnicity.
Risk factors include aging, genetics, repeated spinal strain, smoking, and osteoporosis.
Roughly 75% of those diagnosed will experience periods of worsening symptoms.
Each year, around 5% of asymptomatic individuals may develop symptoms.
The condition most frequently affects the C5-C6 and C6-C7 levels.
Many patients can recover without needing surgery.
Causes
Cervical stenosis can arise fromboth congenital and acquired factors:
01.

Cervical Canal StenosisSymptoms and Clinical Features
Cervical stenosis symptoms vary but often include:
- Pain: Common in the neck, sometimes radiating to the arms or shoulders.
- Radiculopathy Signs:
- Tingling, numbness, or weakness in the arms or hands
- Electric, shooting pain in the arms
- Myelopathy Signs:
- Difficulty walking and balance issues
- Loss of fine motor control
- Weakness in limbs
- Bowel or bladder dysfunction in advanced stages
- Other signs include:
- Reduced neck mobility or stiffness
- Headaches
- Lhermitte’s Sign (electric-shock sensation with neck flexion)
- Symptom progression can be slow, steady, or rapid; some individuals remain symptom-free for years.
Differential DiagnosisCervical stenosis shares symptoms with other conditions, which must be ruled out:
Diabetes-related neuropathy
Inflammatory spinal diseases (e.g., ankylosing spondylitis)
Peripheral neuropathy or vascular disease
Single-level lumbar disc herniation
Spinal cord tumors
Atherosclerosis leads to poor blood flow in the limbs
Diagnosis
and EvaluationDiagnosing cervical stenosis involves:
- Thorough medical history and neurological assessment
- Physical examination
- Imaging:
- MRI: The gold standard for viewing spinal cord compression and other soft tissue changes
- CT scans: Better for assessing bone structures when MRI isn't suitable
- X-rays: Useful in detecting vertebral instability in motion studies
- CT myelography: Alternative if MRI cannot be performed
- Neurological symptom evaluation
- Use of tools such as:
- Neck Disability Index (NDI)
- Neck Pain and Disability Scale (NPAD)
Cervical Canal StenosisConservative Management
For patients without severe symptoms, non-surgical treatment options include:
- Physical Therapy: Improves flexibility, strength, and posture.
- Medications: Anti-inflammatories, pain relievers, muscle relaxants.
- Injections: Epidural steroid injections for pain relief.
- Lifestyle Adjustments:
- Avoiding activities that strain the neck
- Improving workstation ergonomics
- Using a cervical collar for short periods
- Traction Therapy and Patient Education can also be helpful.
- Surgery is reserved for those with worsening neurological function or those who don’t respond to conservative measures.

Role of Physical TherapyA physical therapy program aims to manage pain and improve functionality without altering the anatomy. Treatment usually lasts three months or longer and may include:
Stretching Exercises: Target the neck, arms, trunk, and legs to restore flexibility.
Manual Therapy: Mobilizes cervical and thoracic joints to maintain motion.
Heat Therapy: Increases circulation to relax soft tissues.
Cardio Workouts: Improves stamina and circulation through low-impact exercises.
Aquatic Therapy: Allows pain-free movement in water.
Functional Training: Helps patients manage daily tasks more comfortably.
Additional strategies include:
Targeted muscle strengthening
Postural correction
Scapular stability exercises
Regular position changes
Training in proper lifting, pushing, and pulling techniques
Planning rest breaks during physical activities
Prognosis
Cervical stenosis can significantly impact daily life, potentially leading to chronic pain and reduced mobility. In some cases, severe complications like cauda equina syndrome may occur. Although some patients experience symptom relief over time, most have a gradual decline. The condition can result in long-term disability and place a heavy financial burden on individuals due to ongoing medical costs.