

Our ServicesCervical Myelopathy
Understanding Cervical Myelopathy (C6–C7)
Cervical myelopathy occurs when the spinal cord in the neck region (cervical spine) becomes compressed. This condition can lead to increased muscle tone (spasticity), overactive reflexes (hyperreflexia), abnormal reflex responses, lack of coordination in the fingers or hands, and trouble walking.
The progression of this disorder can vary—some patients experience extended stable periods followed by sudden decline, while others show steady worsening over time. Symptoms depend on the severity and location of the spinal cord compression. If left untreated, cervical myelopathy can eventually lead to major functional loss or even paralysis. Any mass or lesion in the cervical spine capable of putting pressure on the spinal cord can lead to this condition. Common causes include anterior spinal cord compression due to herniated discs, bony overgrowth (spondylotic spurs), ossification of the posterior longitudinal ligament, or spinal stenosis.
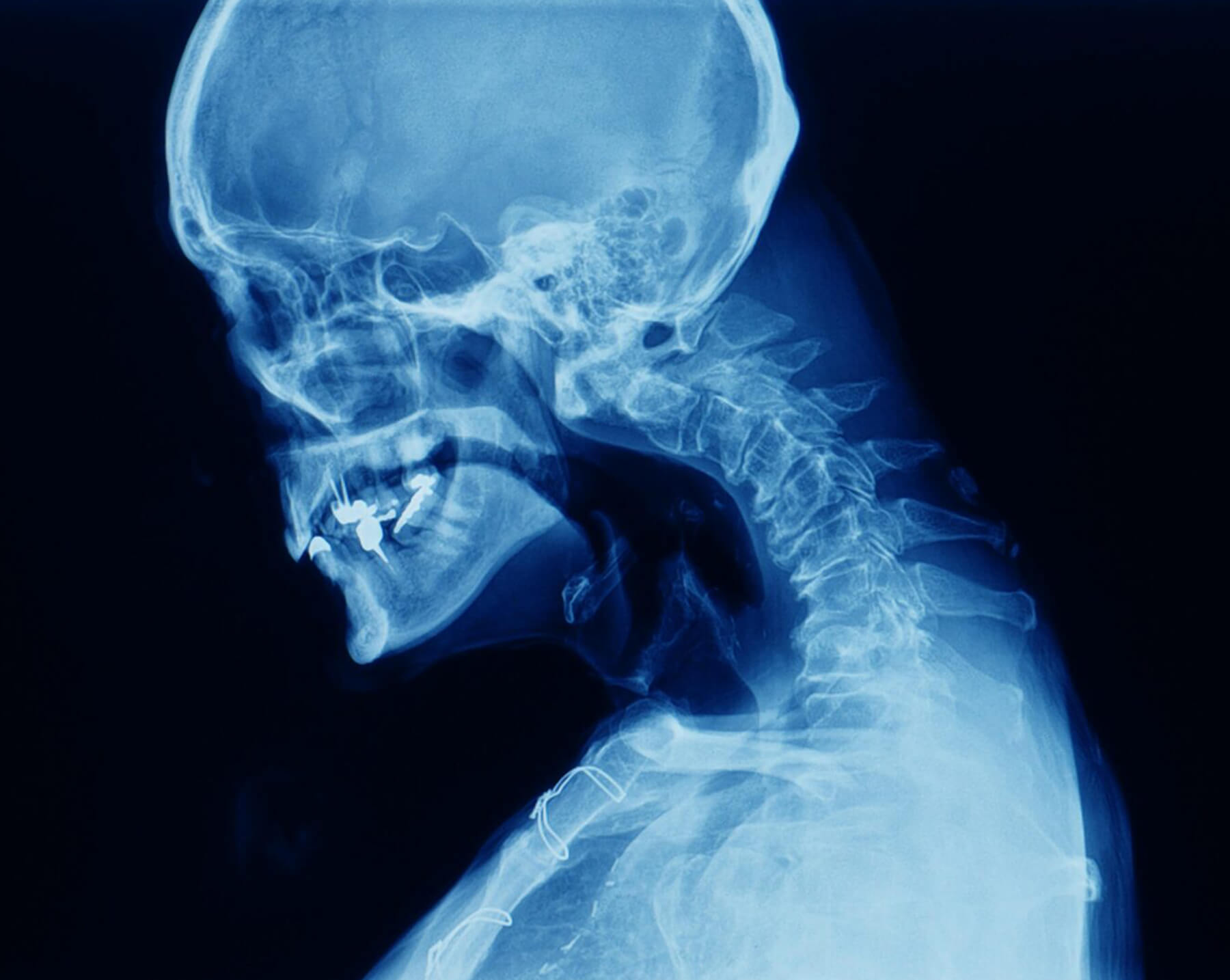
Relevant Cervical Anatomy

The cervical spine consists of seven vertebrae and eight nerve roots. The spinal cord—an essential part of the central nervous system—extends from the brain and passes through the vertebral column starting at the foramen magnum. Because of its critical role, even minor injuries can cause serious complications.
A network of ligaments keeps the cervical spine stable. One such ligament is the ligamentum flavum, which spans between adjacent vertebrae and is connected to the facet joints. Another significant ligament, the posterior longitudinal ligament, runs inside the spinal canal from the second cervical vertebra (axis) to the sacrum and plays a key role in cervical myelopathy.
When conservative  care needs
care needs
a specialist’s touch.
touch.
Epidemiology
Cervical spondylotic myelopathy is the most common spinal cord disorder among individuals aged 55 and above. Degenerative changes in the cervical spine increase with age—about 90% of people over 70, even if symptom-free, show some degeneration. Spinal canal narrowing and cord compression become widespread by the seventh decade. It affects men and women equally, though men may develop it slightly earlier (around 50 years) compared to women (around 60 years). The hospitalization rate is approximately 4.04 per 100,000 person-years.
Causes (Etiology)Cervical myelopathy can stem from multiple factors:
01. Static Factors:
Ischemia to the spinal cord can damage cells like oligodendrocytes, leading to demyelination. Additionally, neurotoxic substances and programmed cell death (apoptosis) can occur.
Cord compression typically results from a mix of constant structural pressure and movement-related (flexion/extension) forces.

Cervical MyelopathySigns and Symptoms
Cervical myelopathy often affects the lateral corticospinal tracts (responsible for voluntary muscle movement) and spinocerebellar tracts (proprioception). Classic symptoms include a spastic, wide-based gait and poor hand coordination.
The condition usually begins subtly in individuals between 50 and 60 years of age. Because it might not cause pain initially, diagnosis can be delayed for years. Symptoms worsen gradually in stages.
Early Symptoms
Numbness, weakness, or pain in the hands
Impaired fine motor skills
Non-specific patterns of weakness and sensory loss
Limited neck movement, particularly during extension
Pain in shoulders or scapula
Paresthesia in arms or hands
Signs of nerve root involvement (radiculopathy)
Neurological signs like Babinski and Hoffmann's reflexes, spasticity, loss of coordination, and bladder/bowel issues
Prognosis worsens if bowel/bladder control is lost or if generalized weakness is present. Complete recovery is rare; most patients experience either stepwise worsening (75%), slow progression (20%), or rapid deterioration (5%).
Key Symptoms
Muscle weakness in the hands
Decreased cervical range of motion
Difficulty with fine motor tasks
Pain in the upper limbs
Balance and gait issues
Overactive reflexes
Sensory disturbances
Nerve root compression signs

Diagnosis
The gold standard for diagnosing cervical myelopathy is a detailed neurological exam combined with MRI. Plain X-rays have limited diagnostic value.
MRI Benefits:
- Identifies spinal canal narrowing, cord compression, and myelomalacia
- Highlights cord compression severity
- Shows T2 hyperintensities in more than half of patients, indicating gray matter involvement
- Offers high accuracy in detecting cervical spinal cord abnormalities
Clinical Testing
Diagnosis is based on physical signs confirmed by imaging. Cook et al. suggest that having three or more of the following increases diagnostic accuracy to 94–99%:
- Gait abnormalities
- Positive Hoffmann's sign
- Inverted supinator reflex
- Positive Babinski sign
- Age over 45
Other helpful clinical tests:
- Spurling’s and distraction tests
- Clonus
- Reflex testing (biceps, quadriceps, Achilles)
- Lhermitte’s sign
- Romberg test
Though these tests may not be highly sensitive individually, combining them enhances diagnostic confidence.
Outcome Assessment Tools
Neck Disability Index
Neck Pain and Disability Scale
Increases circulation to relax soft tissues.
Nurick Score
Japanese Orthopaedic Association (JOA) Score
Cooper Myelopathy Scale (CMS)
European Myelopathy Score (EMS)
Differential Diagnosis
Conditions with similar symptoms includeAdhesive capsulitis
Brown-Sequard syndrome
Carpal tunnel syndrome
Central cord syndrome
Cervical disc disease or strain
Diabetic neuropathy
Multiple sclerosis
Brachial plexopathies (neoplastic or traumatic)
Tumors
Chiari malformation
Guillain-Barré syndrome
Syringomyelia
Osteoporosis
Rheumatoid arthritis
Treatment Approaches
There is no universal agreement on managing mild to moderate cervical myelopathy. Studies show that over two years, surgical and non-surgical treatments yield similar outcomes. Conservative approaches, including physical therapy and anti-inflammatory medications, may offer temporary symptom relief. However, due to the progressive nature of the disease, symptoms typically worsen over time.
Surgical Intervention
Surgery is usually reserved for patients with worsening neurological symptoms or severe cord compression. Surgical treatment is also recommended when the cause is progressive, such as a tumor.
Favorable Surgical Outcomes Are More Likely in Patients Who Have:
- A tingling "electric shock" feeling down their back
- Shorter symptom duration
- Fewer affected spinal segments
- Younger age
- Larger space for spinal cord movement
Surgical Goals:
The main objective is to relieve pressure on the spinal cord. Common procedures include:
- Discectomy or corpectomy (removing parts of discs or vertebrae)
- Laminectomy or laminoplasty (removing or reshaping bone at the back of the spine)
- Fusion surgeries with or without hardware
Early surgical treatment is typically more effective, emphasizing the importance of timely diagnosis.
Post-Surgical Outcomes:
About one-third of patients improve, one-third stabilize, and the remaining third continue to decline despite surgery.
Conservative (Non-Surgical) Management
According to research by Kadaňka et al., patients treated without surgery showed similar long-term results to those who underwent surgery—even after ten years. This supports conservative management as a valid approach for selected cases.

