
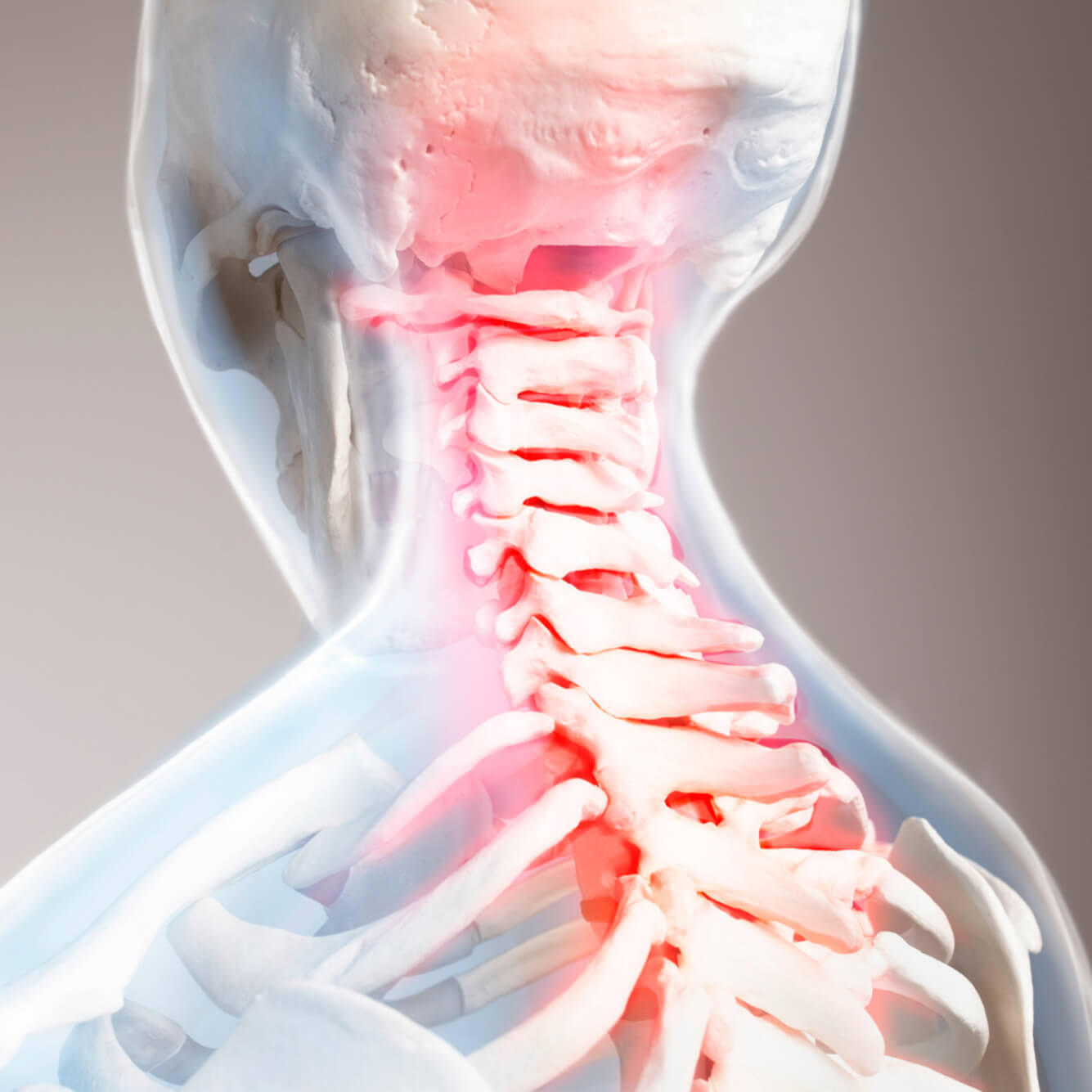
Cervical Spine Infections
The cervical spine, consisting of the uppermost seven vertebrae in the spinal column, plays a vital role in supporting the head and enabling a wide range of motion. While infections in this region are relatively rare, they can be extremely serious and require prompt medical attention. Cervical spine infections, if left untreated, may lead to spinal instability, neurological damage, or even life-threatening complications.
This blog aims to provide a detailed overview of cervical spine infections, covering their causes, signs, diagnostic methods, and available treatment options.

What is a Cervical Spine Infection?
A cervical spine infection refers to the presence of an infectious process affecting the structures of the neck portion of the spine. This can include:

Vertebrae
(osteomyelitis)

Intervertebral discs
(discitis)

Epidural space
(epidural abscess)

Surrounding soft tissues
These infections are typically caused by bacterial, fungal, or—rarely—viral pathogens.
When conservative  care needs
care needs
a specialist’s touch.
touch.
Common Causes and Risk FactorsThe majority of cervical spine infections are bacterial in origin, with Staphylococcus aureus being the most common culprit. Other organisms include:
Mycobacterium tuberculosis (causing spinal TB or Pott’s disease)
Gram-negative bacilli
Fungi (e.g., Candida, Aspergillus) in immunocompromised patients
Risk factors include:
Diabetes mellitus
Immunosuppressive therapy or conditions (e.g., HIV, cancer)
Intravenous drug use
Recent spinal surgery or instrumentation
Chronic infections (e.g., urinary tract infections, dental infections)
Older age

Cervical Spine InfectionsSymptoms to Watch For
Cervical spine infections may start subtly and progress rapidly if not diagnosed early. Common symptoms include:
- Neck pain and stiffness
Often the first and most persistent symptom. - Fever and chills
May indicate systemic infection. - Neurological symptoms
Including numbness, weakness, or tingling in arms and hands due to spinal cord or nerve compression. - Difficulty swallowing or breathing
In rare cases, due to abscess formation or swelling. - Unexplained weight loss and fatigue
More common in chronic or tubercular infections.
DiagnosisEarly and accurate diagnosis is crucial. The following methods are typically used:
Blood tests: Elevated white blood cell count, ESR, and CRP are common.
Blood cultures: To identify the causative organism.
MRI: The most sensitive imaging technique for detecting infections, abscesses, and spinal cord involvement.
CT scan: Helpful in evaluating bone destruction.
Biopsy: Tissue samples may be taken for microbial culture and histopathology.
Treatment Options
Treatment depends on the type, location, severity, and the presence of neurological deficits.01.
Antibiotic Therapy
- Empiric broad-spectrum antibiotics are started early and later tailored based on culture results.
- Treatment duration is usually 6–12 weeks.
ComplicationsUntreated or late-diagnosed cervical spine infections can lead to:
Spinal cord compression and permanent neurological damage
Sepsis
Vertebral collapse and deformity
Chronic pain and disability
Prevention and Outlook
While not all infections can be prevented, controlling underlying conditions (like diabetes), maintaining hygiene during invasive procedures, and prompt treatment of systemic infections can reduce risk.
The prognosis is generally good with early diagnosis and proper treatment. However, delayed care can result in irreversible complications.
Conclusion
Cervical spine infections are serious and potentially life-altering conditions. Awareness of early signs, especially in high-risk individuals, is essential. If you or someone you know experiences persistent neck pain along with systemic symptoms, it is crucial to seek medical evaluation promptly.
Early intervention remains the cornerstone for full recovery and prevention of long-term complications.

