

Our ServicesCervical – Ossification of posterior longitudinal ligament
OPLL is a condition in which bone develops within the posterior longitudinal ligament of the spine.
Epidemiology

This condition is more frequently found in men and tends to affect older individuals. In fact, men are affected twice as often as women.
The prevalence is notably higher in East Asian populations, where about 2.4% are affected, compared to a lower range of 0.2% to 0.7% among Caucasians. In Japan, OPLL is the primary cause of cervical myelopathy.
When conservative  care needs
care needs
a specialist’s touch.
touch.
Related ConditionsOPLL is commonly linked with other musculoskeletal disorders, including:
Diffuse idiopathic skeletal hyperostosis (DISH)
Ossification of the ligamentum flavum
Ankylosing spondylitis
DISH has been found in up to 12% of elderly Caucasian men, and approximately half of those with DISH also have OPLL. This suggests the true prevalence of OPLL in Caucasians may be underreported.

Symptoms
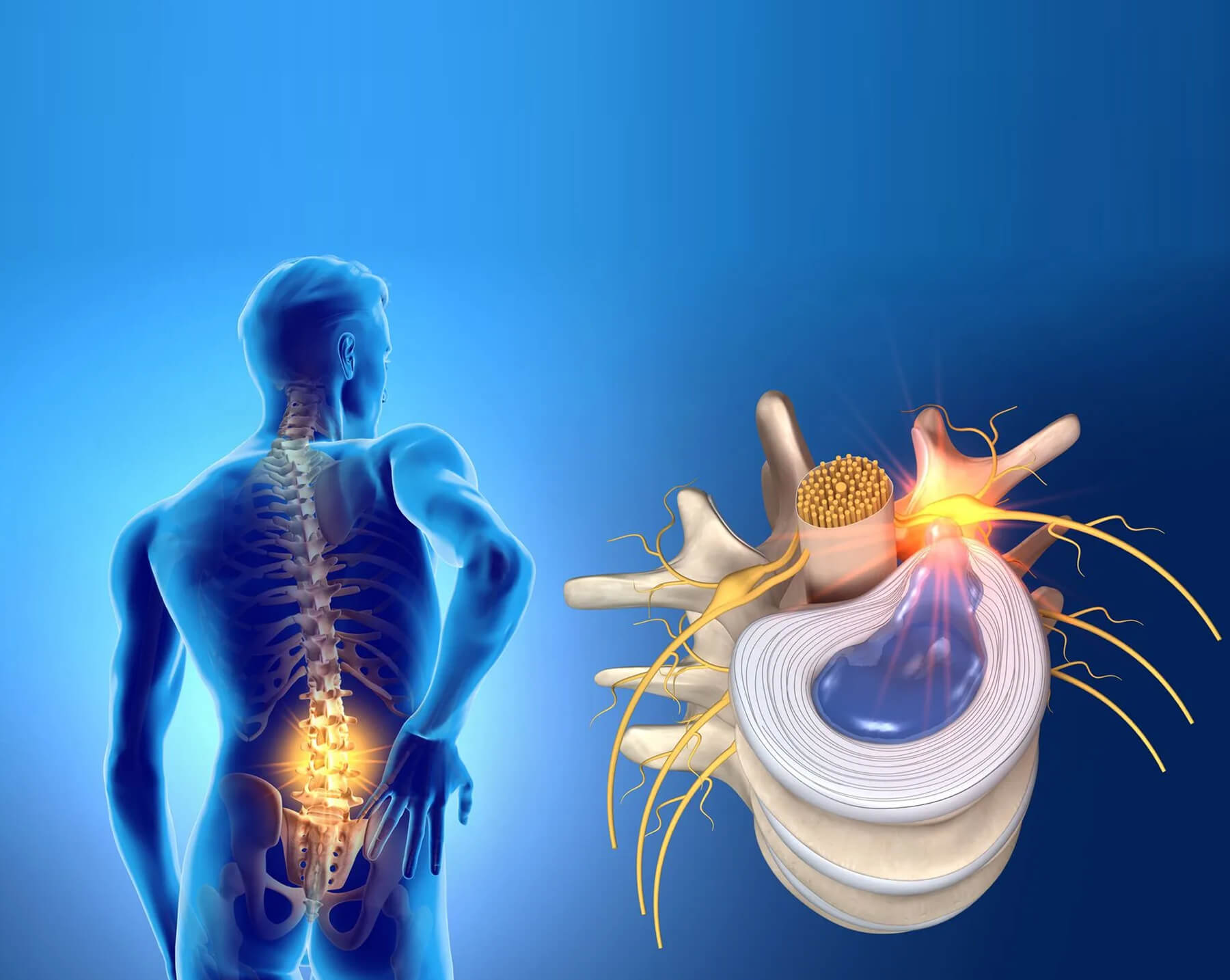
While many patients remain symptom-free, some may show signs of nerve root or spinal cord compression (radiculopathy or myelopathy). These symptoms most often become noticeable between the fourth and sixth decades of life.
Pathogenesis
The precise cause behind OPLL remains unknown.
Common Locations
OPLL most commonly affects the mid-cervical spine and can lead to narrowing of the central spinal canal. This can increase the risk of spinal cord injury, even from minor trauma. The distribution of OPLL cases by spinal region is as follows:
- Cervical spine: 75%
- Thoracic spine: 15%
- Lumbar spine: 10%
Classification
The classification system widely used was developed by Japan’s Ministry of Health, Labor and Welfare, through its Investigation Committee for Ossification of the Spinal Ligaments. It includes:Continuous: Bone formation stretches over several vertebral levels
Segmental: Isolated ossified areas behind individual vertebrae
Mixed: Features of both continuous and segmental types
Localized/Focal: Primarily situated behind an intervertebral disc
Imaging Characteristics
01.
X-rays
Plain radiographs can show OPLL as a linear dense shadow behind the vertebral body, within the front part of the spinal canal.
CT Scans
CT imaging is most effective for identifying OPLL, especially when cervical spinal stenosis is suspected. Ossification may be continuous (extending across vertebrae), segmental (non-continuous), or localized (limited to disc levels). These areas of ossification are often thicker and denser than the surrounding vertebral bone.
Treatment and Outlook
Management options include both non-surgical and surgical strategies. Surgery may involve an anterior, posterior, or combined approach, depending on the case.Anterior approaches (such as multilevel discectomy with plating or corpectomy with fusion) offer direct access to decompress the spinal cord and may yield better improvement in symptoms, though they carry a higher risk of complications in soft tissues.
Posterior approaches (like laminectomy with fusion or laminoplasty) are often better tolerated by older adults.

