

Our ServicesLumbar spine infections
Lumbar spine infections are rare but serious conditions that can lead to significant complications if left untreated. They affect the lower portion of the spine and may involve the vertebrae (bones), intervertebral discs, or surrounding soft tissues. Understanding the causes, symptoms, and treatment options is crucial for early detection and effective management.
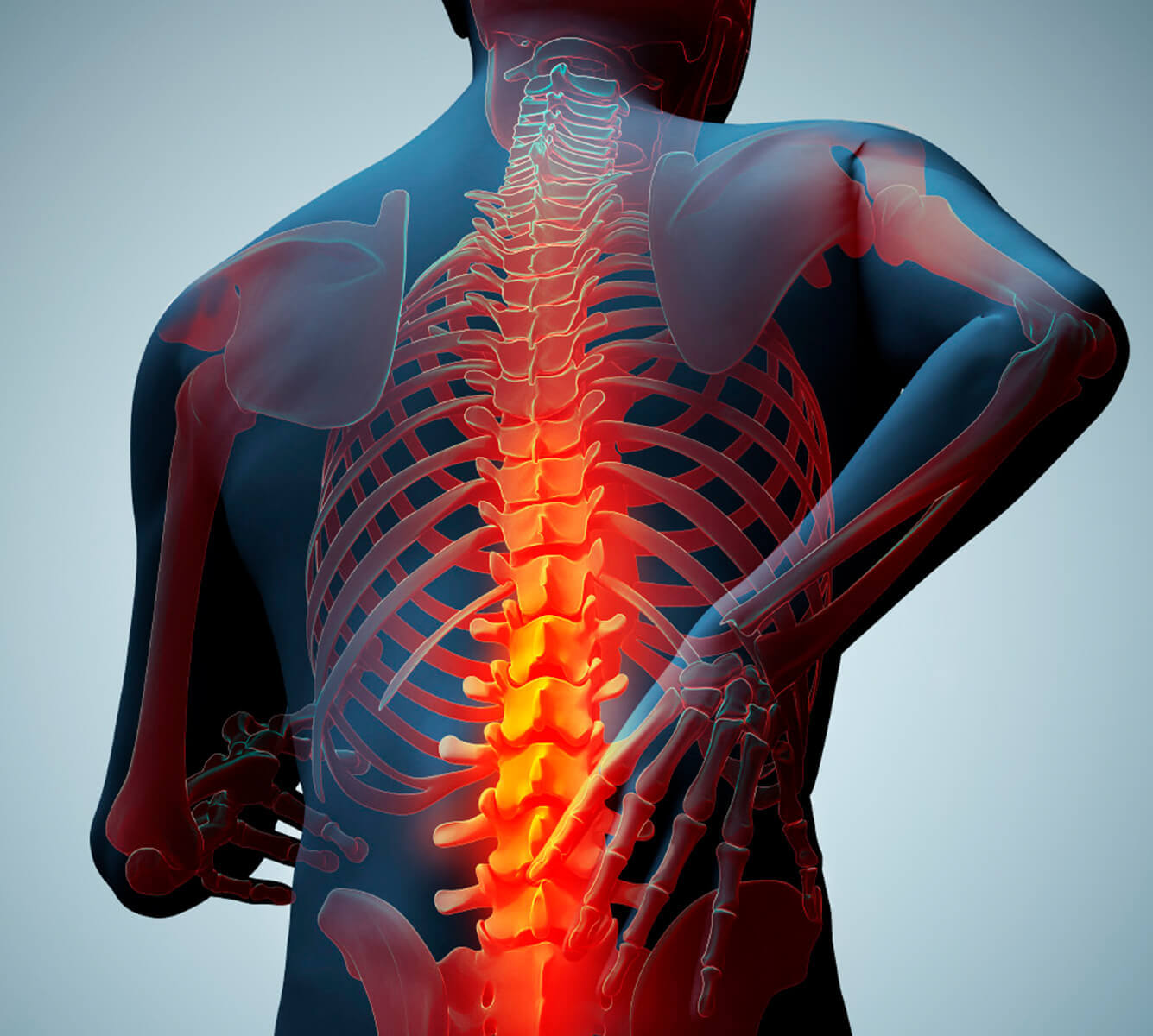
What Is a Lumbar Spine Infection?

A lumbar spine infection, also known as spondylodiscitis, vertebral osteomyelitis, or epidural abscess (depending on the specific area affected), is an infection that occurs in the lower (lumbar) part of the spine. These infections can be bacterial, fungal, or, rarely, viral.
When conservative  care needs
care needs
a specialist’s touch.
touch.
Causes and
Risk Factors
Most lumbar spine infections are caused by bacteria, with Staphylococcus aureus being the most common culprit. Infections can reach the spine through:
- Hematogenous spread (via bloodstream from other parts of the body)
- Direct inoculation during spinal surgery or injections
- Contiguous spread from nearby infected tissues
Risk factors include:
- Weakened immune system (due to diabetes, HIV, cancer, etc.)
- IV drug use
- Recent spinal surgery or instrumentation
- Chronic infections elsewhere in the body
- Elderly age
Common Types of Lumbar Spine Infections
Vertebral osteomyelitis – Infection of the vertebral bones.
Discitis – Infection of the intervertebral disc space.
Epidural abscess – A collection of pus in the epidural space, which can compress the spinal cord or nerves.
Signs and Symptoms
Early symptoms can be vague, often resembling common back pain. However, the pain tends to be more severe and persistent. Key symptoms include:Severe lower back pain
Fever and chills
Night sweats
Unexplained weight loss
Neurological symptoms like numbness, weakness, or difficulty walking (especially if the infection compresses the spinal cord or nerves)
Diagnosis
Prompt diagnosis is essential to prevent permanent damage. Diagnostic tools include:Blood tests – Elevated white blood cells, ESR, CRP
MRI with contrast – The most sensitive imaging technique for detecting spinal infections
CT-guided biopsy – To identify the causative organism
Blood cultures – To determine if the infection has spread systemically
Treatment Options
Treatment depends on the severity and extent of the infection01.
Antibiotic Therapy
- Often the first line of treatment
- Typically administered intravenously for 4–6 weeks, followed by oral antibiotics
- The choice of antibiotics is based on the identified pathogen
Recovery and Prognosis
With timely treatment, many patients recover well, though the healing process can be slow. Delays in diagnosis or treatment increase the risk of complications such as:Chronic pain
Spinal deformities
Permanent neurological damage
Sepsis
Prevention Tips
Proper hygiene during spinal procedures
Prompt treatment of infections elsewhere in the body
Avoiding IV drug use
Regular medical checkups, especially for at-risk individuals
Final Thoughts
Lumbar spine infections are medical emergencies that require a high index of suspicion, especially in patients with persistent back pain and systemic symptoms. Early diagnosis and targeted therapy are key to preventing serious complications and ensuring a successful recovery.

