

Our ServicesCervical Disc Prolapse
Understanding Cervical Disc Prolapse (Cervical Disc Herniation)
Cervical disc prolapse, commonly known as cervical disc herniation, happens when the soft inner core of a spinal disc in the neck pushes through a tear in the tougher outer layer. This protrusion can press on nearby nerves, resulting in symptoms such as pain, numbness, or tingling sensations.
This condition is also referred to by various names, including cervical slipped disc, disc bulge, disc protrusion, prolapsed intervertebral disc, and ruptured or bulging cervical disc.

Anatomy of the Cervical Spine

The spine consists of four main sections—cervical (neck), thoracic (upper back), lumbar (lower back), and sacral (pelvic area)—with a total of 33 vertebrae stacked to form the spinal column.
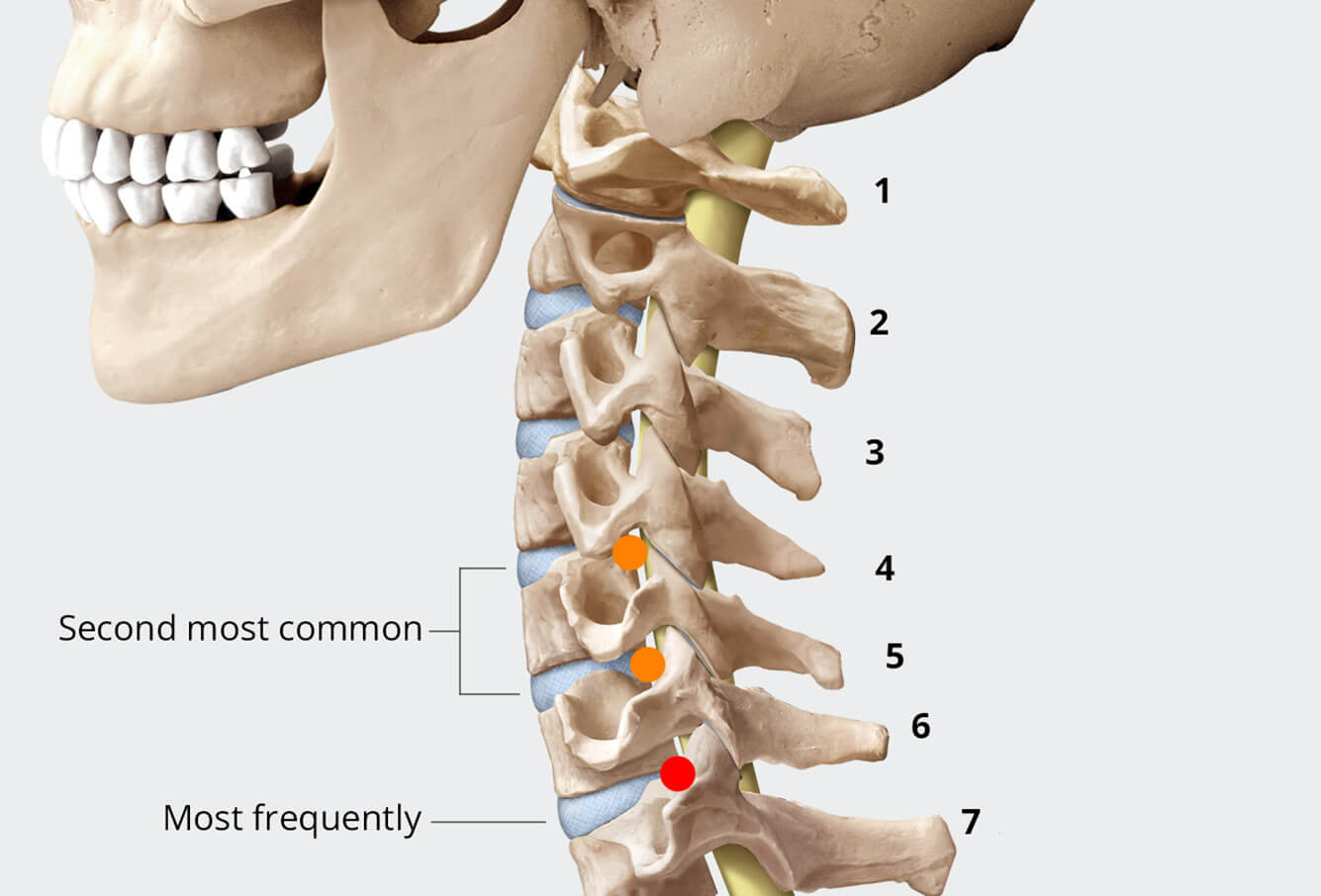
Specifically, the cervical spine contains seven vertebrae, labeled C1 through C7. Disc herniation typically occurs between C5-C6 and C6-C7, often leading to symptoms at the levels of C6 and C7.
When conservative  care needs
care needs
a specialist’s touch.
touch.

How Common is Cervical Disc Prolapse?
Spinal disc herniation is prevalent, even among healthy individuals. Around 20% of younger adults and more than 75% of elderly people have disc herniations, often without any noticeable symptoms. The likelihood of cervical disc herniation increases with age and is especially common in people in their 50s, with a higher occurrence in women (about 60%).
A 2015 Romanian study reported that up to 5.5 people per 100,000 may be diagnosed with cervical disc herniation annually. The most affected vertebrae were C5-C6, followed by C4-C5 and C6-C7.
In Eastern India, a study highlighted various triggers for cervical disc herniation:
- 27.9% of cases were due to trauma such as road accidents within 48 hours.
- 16.1% resulted from lifting heavy loads.
- 11.7% were linked to violence or assault.
- 10.3% were caused by falls.
- 10.3% due to repetitive neck strain.
- 7.3% stemmed from sports or recreational activities.
- 4.4% occurred from objects falling on the head or neck.
- Another 11.7% had no identifiable cause.
Causes of Cervical Disc Prolapse
The most frequent reasons for cervical disc prolapse are disc degeneration and trauma. The cervical spine is more mobile and has smaller discs, making it especially vulnerable to wear and tear.
Additional contributing factors include:
Aging: As we age, the water content in our discs reduces, making them less flexible and more likely to rupture.
Facet joint changes: Degenerative changes around the small joints at the back of the neck can cause disc herniation.
Improper lifting techniques: Lifting with your back instead of your legs can increase herniation risk.
Neck injuries (e.g., whiplash): Sudden trauma can cause the inner disc to push through its outer casing.
Sudden movements: Quick twisting or bending of the neck can stress spinal discs.
Repetitive strain: Activities requiring constant neck bending, lifting, or twisting may gradually damage the spine.
Symptoms of Cervical Disc Herniation
Symptoms vary depending on which disc is affected and which nerve root is compressed. Common signs include:
Neck pain: Can range from mild discomfort to severe pain and may radiate to the shoulders, arms, or hands.
Pain near the shoulder blades, in the arms, or hands
Radiculopathy: Nerve compression can cause tingling, heaviness, weakness, or reduced sensation in the arms or hands.
In rare cases, a severe disc herniation may result in emergencies such as:
Paraplegia: Paralysis in the lower limbs.
Bladder incontinence: Loss of control over urination.
Most patients (around 70%) notice improvements within 4 to 6 weeks, though some may continue to experience mild symptoms over a longer period.
Seek immediate medical attention if you experience:
Visual disturbances (blurred or double vision)
Severe headaches
Vertigo
Facial numbness
Difficulty swallowing or speaking
Significant hand weakness or grip loss
Metallic taste in the mouth
Impaired fine motor control
Unexplained falls or changes in walking
Risk Factors for Cervical Disc Prolapse
Several behavioral and physical factors can raise the likelihood of developing cervical disc issues:
Aging: Disc degeneration is more common in middle age.
Spinal canal abnormalities: Congenital narrowing of the spine may increase susceptibility to damage.
Occupational hazards: Jobs requiring repetitive neck strain, lifting, or twisting.
Trauma: Direct injury to the neck area can lead to disc rupture.
Lack of exercise: Weak spinal muscles increase disc vulnerability.
Smoking: Tobacco use impairs disc health and healing capacity.
Poor posture: Consistent bad posture can stress the cervical spine.
Poor nutrition: Inadequate nutrient intake weakens spinal structures.
Sedentary lifestyle: Minimal movement or prolonged sitting can negatively affect spinal health.
Possible ComplicationsIf not managed properly, cervical disc prolapse may lead to:
- Radiculopathy: Nerve root irritation causing pain and dysfunction.
- Autonomic issues: Irregularities in automatic body functions like urination.
- Hyperreflexia: Exaggerated reflexes due to nerve involvement.
In cases of multilevel degenerative disc disease, the wear and tear of multiple cervical discs may result in:
- Ligamentum flavum hypertrophy: Thickening of spinal ligaments, potentially narrowing the spinal canal (cervical stenosis).
- Cervical myelopathy: Spinal cord compression leading to serious neurological symptoms.

